Table of Contents
The First Ayurveda University in Nepal:
The First University in Nepal Should Have Been an Ayurveda University
Introduction
Ayurveda is deeply rooted in the cultural, medical, and spiritual heritage of Nepal. It has been practiced here for centuries, not merely as a system of medicine but as a way of life. Despite its ancient origins and continued relevance, Nepal has yet to establish a fully dedicated Ayurveda University. This article explores why such a university should have been Nepal’s first, analyzing the historical, social, economic, educational, and health perspectives.
Historical and Cultural Background
Ayurveda has been practiced in Nepal since Vedic times, transmitted through the guru–shishya (teacher–student) tradition, royal patronage, and community-based healing systems.
Despite this rich heritage, modernization and institutionalization of Ayurvedic education have lagged behind.
Without a dedicated university, preservation of ancient texts, proper translation, scientific validation, and systematic research remain insufficient.
Current Situation and Gaps
While Nepal has a few institutions offering BAMS (Bachelor of Ayurvedic Medicine and Surgery), there is no fully specialized academic ecosystem offering postgraduate, doctoral, and interdisciplinary programs.
Research in Ayurveda is fragmented, lacking strong integration with modern scientific methods, clinical trials, and regulatory frameworks.
Standardization of curriculum, clinical protocols, and herbal medicine quality control is still underdeveloped.
Why Nepal Needs an Ayurveda University
Specialized Education and Research – To conduct high-quality research, clinical trials, and academic programs up to PhD level.
Quality Control and Standardization
Establishing national standards for Ayurvedic curriculum, clinical practice, and medicine manufacturing.
Conservation of Medicinal Plants
Sustainable harvesting, cultivation, and biodiversity protection.
Integration with Modern Medicine
Developing evidence-based integrative healthcare models.
Public Health Contribution
Utilizing Ayurveda’s preventive approach to combat non-communicable diseases (NCDs).
Employment and Economic Growth
Training skilled professionals for healthcare, research, herbal industry, tourism, and entrepreneurship.
Expected Benefits
Short-Term (1–3 years)
Revised, standardized Ayurvedic curriculum.
Increased number of trained Ayurvedic physicians and researchers.
Initiation of herbal medicine quality testing.
Long-Term (3–15 years)
Internationally recognized research and publications.
Ayurveda-based public health models for NCD prevention.
Growth of herbal pharmaceutical industry and health tourism.
Preservation and promotion of Nepal’s cultural and medicinal heritage.
Proposed Structure of the University
Faculties:
Ayurvedic Pharmaceutics and Rasashastra
Public Health and Preventive Medicine
Medicinal Plant Conservation and Botany
Integrative Medicine
Ayurveda Lifestyle and Mental Health Sciences
Programs:
Undergraduate: BAMS (with updated evidence-based modules)
Postgraduate: MD/MS in various Ayurvedic specialties
Doctoral: PhD and Post-Doctoral programs
Diplomas/Certificates: Ayurvedic Pharmacy, Herbal Farming, Ayurveda Lifestyle Coaching, Clinical Research
Research Centers:
Clinical Trial Center
Pharmacopoeia and Quality Control Laboratory
Herbal Conservation and Biotechnology Unit
Integrative Medicine Center
Curriculum and Quality Assurance
The curriculum should combine classical Ayurvedic principles with modern biomedical sciences, ethics, research methodology, and public health.
Accreditation by national and international bodies should be mandatory.
Clinical practice should follow evidence-based protocols with proper documentation.
Human Resource Development
Recruitment of highly qualified national and international faculty.
Faculty training programs and academic exchange partnerships.
Research fellowships and grants for young scholars.
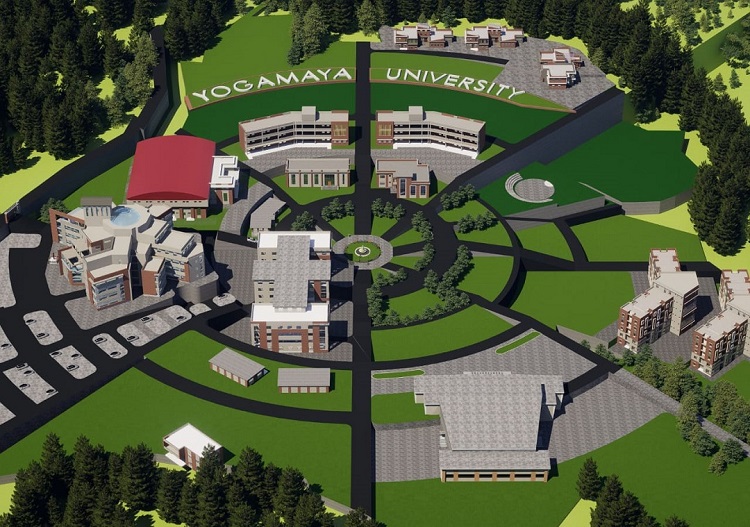
Infrastructure Requirements
Main campus with teaching hospital, research laboratories, herbal gardens, and pharmaceutical production units.
Digital library and e-resources.
Biosafety and advanced clinical trial facilities.
Policy and Legal Framework
Government policy support and legislative approval for the university’s establishment.
Clear regulations for herbal pharmacovigilance, intellectual property rights (IPR) for traditional knowledge, and benefit-sharing mechanisms.
Official recognition by the National Education Commission and health authorities.
Financial Planning
Initial Funding:
Government grants, international aid, and Public–Private Partnerships (PPP).
Long-Term Sustainability:
Tuition fees, clinical services, herbal product sales, research grants, and medical tourism.
Collaboration with WHO, UNESCO, and global research bodies.
Challenges and Risks
Political and Administrative Barriers: Need for strong political commitment.
Scientific Validation Gaps: Without rigorous testing, acceptance in global academia will be limited.
Human Resource Shortage: Need to develop highly trained specialists.
Financial Constraints: Sustained investment required.
Implementation Roadmap
Phase I
Feasibility and Planning (0–6 months)
Needs assessment, site selection, and policy consultation.
Phase II
Policy Approval (6–12 months)
Drafting of University Act, budget approval, and initial governance structure.
Phase III
Infrastructure and Staffing (1–3 years)
Campus and hospital construction, faculty recruitment, launch of BAMS and MD programs.
Phase IV
Research and Expansion (3–5 years)
Launch of PhD programs, clinical research collaborations, herbal product development.
Phase V
Global Recognition and Sustainability (5+ years)
International student enrollment, large-scale exports, and health tourism integration.
Stakeholders and Collaboration
Government:
Ministries of Health and Education.
Communities:
Traditional healers, herbal farmers, indigenous knowledge holders.
Academia:
International universities and research bodies.
Private Sector:
Pharmaceutical companies, herbal product manufacturers, wellness tourism operators.
Civil Society:
NGOs and consumer groups.
Ethical and Socio-Cultural Considerations
Protection of indigenous knowledge through IPR.
Inclusion of women and marginalized communities in education and leadership roles.
Transparent community consent in research and resource utilization.
International Opportunities
Potential for global recognition and student recruitment.
Export of Ayurvedic medicines and health tourism services.
Challenges include maintaining scientific credibility and quality assurance.
Conclusion and Recommendations
Establishing an Ayurveda University in Nepal is not just a matter of academic growth—it is a cultural, economic, and healthcare necessity. Such a university could have been Nepal’s first, given our rich heritage and the global demand for holistic healthcare.
Key Recommendations:
Form a high-level task force to conduct a feasibility study.
Implement a Public–Private Partnership model in the initial phase.
Integrate traditional wisdom with modern science in curriculum design.
Ensure biodiversity conservation and sustainable herbal resource use.
Establish independent accreditation and evaluation systems.
The First Ayurveda University in Nepal The First Ayurveda University in Nepal The First Ayurveda University in Nepal The First Ayurveda University in Nepal The First Ayurveda University in Nepal The First Ayurveda University in Nepal The First Ayurveda University in Nepal The First Ayurveda University in Nepal The First Ayurveda University in Nepal The First Ayurveda University in Nepal The First Ayurveda University in Nepal